- Share
- Share on Facebook
- Share on X
- Share on LinkedIn
The Sleep Apnea Syndrom : SAS

There exist several sleep pathologies and they can affect at any age of life. Some of them are very frequent and have important consequences in terms of morbidity, social and medico-economic consequences. From this perspective, the Sleep Apnea Syndrome (SAS) is one of the major pathologies, affecting more than 15% of the global population.
Taking the SAS into account for last 30 years lead to :
- a better understanding of the pathology occurrence causes as well as the involved biological mechanisms,
- an apprehension of the associated complications, especially cardiovascular complications and the resulting morbidity.
What is an OSAS?
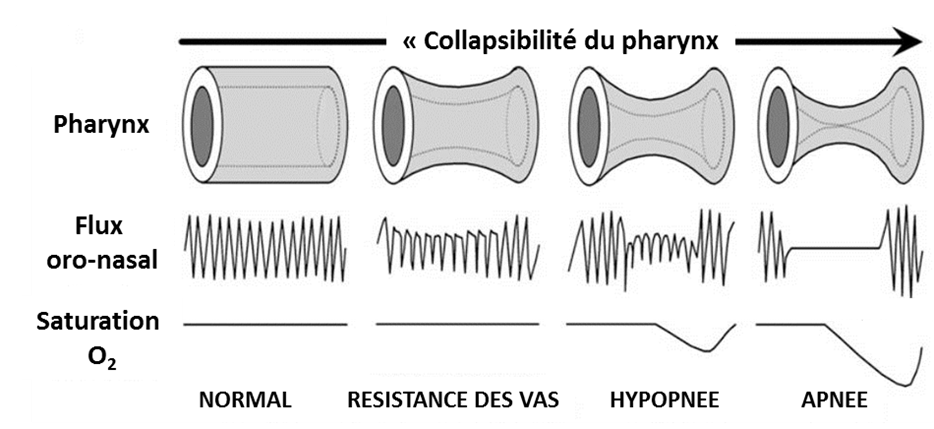
An Obstructive Sleep Apnea Syndrome (OSAS) is identified when the pharynx repeatedly collapses during the sleep, generating a more or less important upper airways obstruction, due to a pharynx anatomical shrinkage (back of the throat).
Causes:
The upper airways opening depends on several factors. When breathing in, the negative intra-thoracic pressure generated by the inspiratory muscles (especially the diaphragm) is likely to induce an pharynx upper airway collapse. On the opposed, the pharynx dilatory muscles counteract this collapse and keep the upper airways open during the breathing in. A collapse occurs when there is an imbalance between the pharynx dilatory muscles contraction generated strength and the negative inspiratory pressure.
The OSAS physiopathology is multy-factorial and includes a loss of dilatory muscles capacity to keep the pharynx open during the slumber (rise of the ''collapsibility'') and an anatomical reduction of the upper airways diameter. This reduction is induced by various factors, such as maxillo-facial abnormalities, obesity, or the redistributing in the neck of the excess of liquid that was accumulated during the day (very common in patients with hydrosodic retention).
Consequences:
There are three major consequences for these pharynx repeated collapses:
- rise of the breathing effort,
- micro-awakening occurrence ending the breathing events,
- arterial blood desaturation-reoxygenation sequences occurrence
These desaturation-reoxygenation sequences repeat are the intermittent hypoxia, now accepted as being the OSAS metabolic and cardiovascular complications major cause.
Diagnostic:
There are multiple SAS suggestive clinical signs. Among them, the first clinical event is a diurnal somnolence linked to the sleep disruption (with the respiratory events-induced micro-awakening). The apneic patient shows other signs such as snoring, awakening headaches, chronic asthenia, libido fall, mood troubles, cognitive dysfunction, or cardiovascular (hypertension, heart diseases, heart failure, atrial fibrillation) and/or metabolic (metabolic syndrome, type 2 diabetes) pathologies. These symptoms can often be under-estimated by the patient. Given that is is usually the partners who is able to hear the snoring, the relatives then play a crucial role for an SAS suspicion
Treatement:
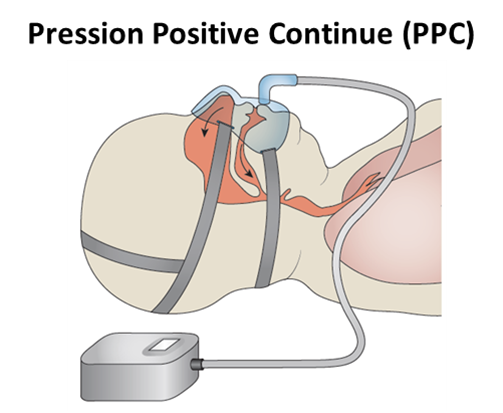
The first step in an SAS therapeutical care is to introduce the patient to hygieno-dietetic rules such as weight loss, alcohol and sedatives eviction, or a regular physical activity practice. This physical activity practice contributes to better sleep quality and a decrease of the liquid redistribution in the neck (hydrosodic retention improvement). These lifestyle modifications can limit the apneas and/or some of the consequences. However, the reference treatment being a continuous positive airway pressure (CPAP) administration, nasally delivered during the sleep.
This technique maintains the upper airways open, eliminating the apneas and normalizing the sleep. The life quality is then improved in 80% to 100% of the observed patients. The CPAP generates a neuro-cognitive functions enhancement and a cardiovascular risks prevention. Nevertheless, CPAP unwillingness and waiver rates can reach up to 40% of the patients and CPAP does not improve all OSAS-linked complications, especially when it is linked to other co-morbidities. Depending on the SAS etiology, a mandibular advancement splint is proposed. This splint is worn at night and moves the mandibles forward and thus the tongue and the soft palate, liberating the pharynx and limiting the obstruction occurrence. Its efficiency rate is about 60%.
Finally, in some specific cases (and most in an CPAP intolerance case), surgery is considered, such as uvulopalatopharyngoplasty, tonsillectomy, basic tongue surgery, hoyïdial surgery, and bimaxillar osteotomy, all with the objective of a pharynx opening.
- Share
- Share on Facebook
- Share on X
- Share on LinkedIn